Use of mobile app to enhance functional outcomes and adherence of home-based rehabilitation program for elderly with hip fracture: A randomized controlled trial
Abstract
Background: Mobile app has been used to improve exercise adherence and outcomes in populations with different health conditions. However, the effectiveness of mobile app in delivering home-based rehabilitation program to elderly patients with hip fracture is unclear.
Objective: The aim of this study was to test the effectiveness of mobile app in delivering home-based rehabilitation program for improving functional outcomes and reducing caregiver stress with enhancing adherence among the elderly patients with hip fracture.
Methods: A randomized controlled trial with an intervention period of two months was performed. Eligible participants were randomized into either experimental group with home-based rehabilitation program using a mobile app or control group with home-based rehabilitation program using an exercise pamphlet. Primary outcomes were Modified Functional Ambulatory Category (MFAC), Elderly Mobility Scale (EMS) and Lower Extremity Functional Scale (LEFS). Secondary outcomes were exercise adherence and Modified Caregiver Strain Index (M-CSI). The outcomes were collected at pre-discharge training session, one month and two months after hospital discharge.
Results: A total of 50 participants were enrolled, with 19 participants in the experimental group and 20 participants in the control group. Eleven participants had withdrawn from the study. The experimental group showed higher exercise adherence than the control group in first month (p=0.03). There were no between-group differences in MFAC, EMS, LEFS and M-CSI at the first month and second month.
Conclusion: Use of the mobile app improved exercise adherence, yet it did not improve physical performance, self-efficacy and reduce caregiver stress when compared to a standard home rehabilitation program for elderly patients with hip fracture. Further studies to investigate the benefits of mobile apps are required. (ClinicalTrials.gov ID: NCT04053348.)
Introduction
About half of women and a quarter of men suffer from a fragility bone fracture in their lifetime,1,2 which is mostly associated with fall.2 Hip fracture is commonly seen among all fragility fracture cases and it places an increasing burden on healthcare service providers around the world. A global estimation on the number of hip fractures in 2050 is between 7.3 million and 21.3 million,3 and over half of them will occur in Asia due to the higher growth of ageing population in many Asian regions.4 A 2015 study showed that there was a steady increase in the incidence of geriatric hip fracture in Hong Kong.5 Assuming no increase in age-specific rates, the estimated annual incidence of elderly hip fracture in 2040 is more than 14,500.5
Previous studies showed that post-fracture limitations, such as impaired balance,6 decreased mobility and lower limb strength,6,7 restrained elderly patients with hip fracture from participating in daily activities to live independently and safely.6,8 Functional performance of these patients was greatly affected by these limitations. More than half of them failed to regain pre-fracture functional abilities two years after injury and they have a moderate-to-high risk of further falls.8,9 Main factors affecting functional performance were pre-fracture ambulatory level and age.10 Post-fracture limitations also increase the burden of informal caregivers, who are responsible for providing assistance to patients in performing their daily activities safely. A study reported that 50% and 26% of caregivers perceived a high level of caring stress at one month and one year after the patients were discharged from hospital, respectively.11 Factors influencing caregiver stress level, such as pre-fracture functional level, caregiver–patient relationship and age of patients, were also identified in the study.11
Provision of educational materials, which consist of home exercises and caring skills, is essential for patients and caregivers to take responsibility and manage their conditions at home. Adherence to home exercises has been shown to be associated with improved patient outcomes.12,13 Educational materials are conventionally delivered through paper handouts, which are reliable and convenient for distribution. However, written texts and illustrations could be incomprehensible, leading to a decrease in patients’ exercise adherence at home.14 Other possible factors, such as self-efficacy, age and perceived social support from family, were shown to be associated with exercise adherence.15
Use of mobile apps in exercise education was shown to improve exercise knowledge and self-efficacy when compared with the use of paper handouts.16 Some researchers have therefore directed their attention in evaluating the strategy of using technology to improve patients’ exercise adherence and outcomes. Recent randomized controlled trials (RCTs) reported greater adherence to home programs, which were delivered with an Internet-based self-monitoring system via mobile phones, in patients with hemophilia-related knee dysfunction and musculoskeletal conditions, respectively.17,18 Promising results were also reported with the use of mobile apps to improve adherence and outcomes in other health areas, such as weight loss and diabetic management.19,20 However, elderly patients may find difficulties in using mobile apps and experience usability issues, such as limited screen size of mobile devices and complicating app interactions.21 Successful application of mobile apps in populations with different health conditions may not be transferable to geriatric populations with hip fracture. Thus, a joint research team with the collaboration among Physiotherapy Department of Tai Po Hospital (TPH) in New Territories East Cluster (NTEC), Hong Kong Polytechnic University Rehabilitation Science (HKPURS) Department and NTEC Information Technology Department was formed to conduct a study to test the effectiveness of mobile app in delivering home-based rehabilitation program for improving functional outcomes and reducing caregiver stress with enhancing adherence among the elderly with hip fractures.
The study’s primary hypothesis is that the home-based rehabilitation program delivered using mobile app will result in better functional outcomes compared to usual care delivered using the conventional paper handouts. Secondary hypothesis is that mobile app intervention will result in better adherence and lesser caregiver burden.
Method
Study design
It was a parallel, two-arm (experimental control), RCT with a two-month intervention period (see Fig. 1).
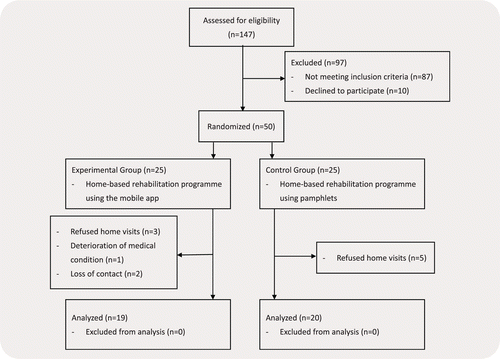
Fig. 1. Flow diagram of trial.
Participants
All patients were recruited from the inpatient Geriatric Hip Fracture Rehabilitation Program in the Department of Orthopaedic Rehabilitation (DOR) of Tai Po Hospital. Tai Po Hospital is a tertiary-care hospital and it provides rehabilitation services to hip fracture patients who are transferred from acute hospitals in the New Territories East Cluster. To be eligible for enrolment, patients fulfilled the following inclusion criteria: (1) have a primary diagnosis of hip fracture; (2) be 60–90 years old; (3) be literate enough to read and understand simple questions in Chinese; (4) be discharged home and taken care by caregiver; (5) have at least category three measured by the Modified Functional Ambulatory Category (MFAC) upon discharge; (6) have access to a smartphone or tablet (iOS or Android platform); (7) have signed the written informed consent. The exclusion criteria were as follows: (1) have a bilateral hip fracture or hip fracture is the result of a malignancy; (2) have significant cognitive deficits with a score of less than 19 in Hong Kong Version of Montreal Cognitive Assessment (HK-MoCA)22; (3) have significant cardiopulmonary contraindications or pre-existing conditions that preclude participation in an exercise program; (4) have a terminal illness (survival expected to be less than one year); (5) have severe visual deficits or legally blind.
Based on the power being set at 0.80, type-1 error α of 0.05 and previous similar studies,23,24 the sample size needed in this design to run two-way repeated measures analysis of variance (ANOVA) was 126 (63 participants per group). This sample achieved 80% power to test the main effect if Geisser–Greenhouse Corrected F-test was used with a 5% significance level and an effect size of 0.42. It also achieved 82% power to test the interaction effect if Geisser–Greenhouse Corrected F-test was used with a 5% significance level and an effect size of 0.41. With the consideration of possible drop-out of the participants (an estimated 15% attrition), a total of 144 participants (72 participants in each group) should be recruited for the whole study.
Potential participants were identified by case physiotherapists a week before discharge and these participants received brief information about the study. Research team members approached the participants who agreed to be contacted for further explanation of the study. A written informed consent was obtained from each participant before enrolment. Once enrolled, case physiotherapists assessed the participants to collect baseline characteristics. The participants were then allocated to either experimental group or control group using a computer-generated randomization sequence. Ethical approval was obtained from the Joint Chinese University of Hong Kong–New Territories East Cluster Clinical Research Ethics Committee before start of the study.
Potential risk and preventive measures
All participants recruited were screened by physiotherapists according to the exercise prescription guidelines of the American College of Sports Medicine (ACSM) for any contraindications.25 Suitability of participating in home exercise programs was assessed by physiotherapists based on environmental risk, fall risk and competence of participants or caregivers in performing home exercises. Participants should have sufficient space and appropriate supporting furniture at home for performing the exercises. Both participants and caregivers should also have a good understanding of prescribed exercises so that participants could perform the exercises safely. Caregivers should be able to supervise patients in performing home exercises.
Intervention
A briefing session was arranged for all participants with their caregivers before hospital discharge. This session included provision of home-based rehabilitation program and caregiver education by case physiotherapists. For participants and caregivers in the experimental group, they were instructed to install the mobile app in the participants’ mobile devices. A smart tablet (240mm × 169.5mm), which also had the mobile app installed, could be loaned to those participants without any suitable mobile devices. They learnt how to operate the mobile app and perform exercises along with exercise videos embedded in the app. For participants and caregivers in the control group, they received an exercise pamphlet and a caregiver skill pamphlet instead of the mobile app. The pamphlets consisted of written texts and printed illustrations. Both groups received the same home-based rehabilitation program and caregiver skill information. The caregiver education involved demonstration on assisting patient in transfer and ambulation (Table 1). Physiotherapists assessed the participants during the briefing session and if there were any tasks that required assistance to complete safely, physiotherapists would instruct the caregivers to view the corresponding educational material in the mobile app or pamphlet.
| Category | Task |
|---|---|
| A. Patient Transfer | From lying to sitting From sitting to standing Bed-to-chair transfer |
| B. Patient Ambulation | Level ground walking Stairs walking |
The home-based rehabilitation program for hip fracture patients involved a combination of training focused on strength, coordination and functional movements of geriatric hip fracture patients. All exercises in the rehabilitation program were safe for patients who underwent different hip fracture operations. There were four levels of difficulty, consisting of four–six exercises in each exercise level (Table 2). Participants were instructed to perform the prescribed level of exercises once per day with the course length varying from 20min to 30min. The progression level of the exercise program was reassured by the domiciliary physiotherapists during weekly home visits based on clinical performance of the participants. To ensure safety in performing home exercises without a physiotherapist, participants were required to perform the prescribed exercises correctly in the briefing session. Literacy of the caregivers was also assessed by physiotherapists. They were required to demonstrate the use of mobile app or exercise booklet, and explain the prescribed exercises to physiotherapists at the end of the briefing session.
| Levels of difficulty | |||||||
|---|---|---|---|---|---|---|---|
| Exercise item | Equipment needed | Training side | Dose | 1 | 2 | 3 | 4 |
| 1. Knee extension in sitting (resistance∗) | Resistance band | Both | Ten repetitions for two sets | √ | √ | √ | √ |
| 2. Ankle plantarflexion in sitting (resistance∗) | Resistance band | Both | Ten repetitions for two sets | √ | √ | √ | √ |
| 3. Sit-to-stand (assisted) | Table | Both | Ten repetitions for two sets | √ | |||
| 4. Sit-to-stand (aided) | Table | Both | Ten repetitions for two sets | √ | |||
| 5. Sit-to-stand (unaided) | Table | Both | Ten repetitions for two sets | √ | |||
| 6. Knee flexion in standing | Table | Both | Ten repetitions for two sets | √ | |||
| 7. Hip abduction in standing | Table | Both | Ten repetitions for two sets | √ | |||
| 8. Hip abduction in standing (resistance∗) | Table + Resistance band | Both | Ten repetitions for two sets | √ | √ | ||
| 9. Mini-squat | Table | Both | Ten repetitions for two sets | √ | |||
| 10. Lunge | Table | Both | Ten repetitions for two sets | √ | √ | ||
| 11. Toe and heel raise in standing | Table | Both | Ten repetitions for two sets | √ | |||
| 12. Hip marching in standing | Table | Both | Thirty repetitions for two sets | √ | |||
Mobile app development and features
A steering group including physiotherapists, informatics and university research experts was formed to co-design the app, formulate the study design and compose educational content for the patients. Meetings were also held with all involved clinicians to refine the mobile app before study commencement.
The mobile app was developed to facilitate the implementation of a home-based rehabilitation program. Participants could use this mobile app to follow home-based exercises prescribed by their physiotherapists, track their exercise progress and obtain relevant information about hip fracture rehabilitation. Their caregivers could also refer to this information to learn about how to assist their care receivers. The features of the mobile app include the following:
| (1) | Exercise program: Preloaded exercises at four different levels of difficulties for the geriatric hip fracture patient (Table 2). | ||||
| (2) | Progress summary: It allows patients to see their progress and ultimately improve their self-efficacy through completion of tasks. A summary of the rehabilitative exercises completed by the patient will be presented in calendar format for easy interpretation. | ||||
| (3) | Push reminder: It alerts the participants to follow the exercise schedule and sends out motivational message to encourage them. | ||||
| (4) | Rehab knowledge: It allows participants and their caregivers to obtain knowledge on post-hip fracture management including the related surgical intervention, post-operative management and precautions. | ||||
| (5) | Caregiver skill: Video libraries of a wide range of practical skills and information about taking care of geriatric hip fracture patient for the caregivers. | ||||
| (6) | Support information: Useful online health information and supporting resources for participants and caregivers. | ||||
Outcomes
Demographic data of the patients including age, gender, post-operation duration and length of hospital stay was collected upon discharge. Assessments on specific outcomes were conducted at pre-discharge training session (T0) by the case physiotherapists, first month (T1) and second month (T2) post-discharge by domiciliary physiotherapists during home visits. There were three primary and two secondary outcomes.
Primary outcomes
Modified functional ambulatory category
The MFAC is a seven-point Likert scale to classify a patient’s walking capacity. Gait is divided into seven categories, ranging from no ability to walk and requires manual assistance to sit or is unable to sit for 1 min without back or hand support (MFAC 1) to the ability to walk independently on level and non-level surfaces, stairs and inclines (MFAC 7).26 The inter-rater reliability of MFAC [the intraclass coefficient (ICC)] was 0.982 (0.971–0.989), with a kappa coefficient of 0.923 and a consistency ratio of 94% for the stroke patient. The ICC of MFAC in patients with hip fractures was 0.96.26
Elderly mobility scale
The Elderly Mobility Scale (EMS) was used to assess an individual’s mobility problems through seven functional activities including lying, sitting, standing and walking.27 The possible total score is 20. Patients receiving a score under 10 indicate that they are dependent on mobility and activities of daily living (ADL). Patients receiving a score between 10 and 13 indicate that they are marginal in terms of safe mobility and independent in ADL. Patients receiving a score over 14 indicate that they are able to perform mobility and ADL independently and safely. EMS demonstrated good inter-rater reliability and concurrent validity.28
Lower extremity functional scale
Lower Extremity Functional Scale (LEFS) is a 20-item questionnaire intended to measure patients’ functions with a wide range of lower extremity conditions.29 Each item is rated on a five-point scale (0 = extreme difficulty or unable to perform activity, 4 = no difficulty); total scores range from 0 to 80, and lower scores represent greater difficulty. It has been shown to be highly reliable, correlates with other constructs and is an independent predictor of the patient and physician’s assessment of change in patients.29 The minimal clinically important difference (MCID) for the LEFS is nine points.29 This questionnaire has been validated in Taiwan-Chinese version.30
Secondary outcomes
Exercise adherence
Adherence to the prescribed home-based rehabilitation program was collected in both groups at the first month (T1) and second month (T2) after discharge using exercise logs. Participants were asked to record their exercise logs either by the use of the mobile app for the experimental group or by exercise diaries provided for the control group. Collected exercise logs were used to calculate the percentage of the number of exercise sessions completed to the number of exercise sessions prescribed in the two-month period.
Modified caregiver strain index
The original version of the Caregiver Strain Index (CSI) was developed in 1983. It was designed to detect the physical, psychological, social and financial strain of the informal caregiver. It consisted of 13 items. There were only two options for the respondent to choose (score 1 if the respondent chose “yes”, otherwise score 0 if the respondent chose “no”). The CSI was modified later in 2003. Some of the items were rephrased and one option category (yes, sometimes) was added. There were three option categories for the respondents to choose and the score ranged from 0 to 26. Caregivers would face a high level of strain with high CSI score. The modified version of CSI [i.e. the Modified Caregiver Strain Index (M-CSI)] achieved a high internal reliability (α=0.90).31 Chan et al. examined whether M-CSI was still valid when it was applied on the Hong Kong Chinese caregivers in 2013. They validated the Chinese version of the Modified Caregiver Strain Index and the results showed that it achieved a good internal reliability (α=0.91).32
Data analysis
Independent t-test and Pearson’s Chi-square test were used to compare the baseline characteristics between the two groups. One-way repeated measures ANOVA was conducted to see the within-group differences at different assessment occasions. If there was a significant difference within a group, a post-hoc paired t-test would be conducted to evaluate this within-group difference. Additionally, a two-way repeated measures ANOVA was used to find out if there was any significant interaction effect between the two groups across different assessment occasions. If there was a significant effect between the two groups, a post-hoc independent t-test would be carried out with Bonferroni correction. All statistical analyses were performed using the IBM SPSS program version 28 for Windows; the significance level was set at p<0.05.
Results
From October 2019 to March 2021, 50 participants were recruited and randomized into experimental and control groups. Eleven participants withdrew from the study, with eight participants refusing home visits, one participant having deterioration of medical condition and two participants being unable to contact. There were no adverse events that occurred as a result of participation. The proposed sample size of 144 participants was unable to be achieved in this study due to a significant decrease in the number of eligible participants in the hospital after the outbreak of COVID-19. High drop-out rates of participants due to refusal of home visits were observed. Thirty-nine participants completed the study and data was collected for analysis, including 19 participants in the experimental group and 20 participants in the control group. Data normality was checked using the Shapiro–Wilk test. Since the test results suggested non-normality, non-parametric tests for data analysis were adopted. Mann–Whitney U-test and Pearson’s Chi-square test were used to compare the baseline characteristics between the two groups. Friedman test was conducted to see the within-group differences at different assessment occasions. If there was a significant difference within a group, post-hoc Wilcoxon signed-rank test would be carried out with Bonferroni correction. Mann–Whitney U-test was used to compare the between-group differences. For all participants in both groups, the mean age was 77.4 years and the percentage of males was 51.3%. As shown in Table 3, there were no significant differences in the baseline characteristics of participants between the experimental and control groups.
| Participants’ characteristics | Experimental group (n = 19) | Control group (n=20) | p-Value (Mann–Whitney U) | p-Value (Chi-square) |
|---|---|---|---|---|
| Age (years), mean (SD) | 75.8 (7.2) | 79 (8.8) | 0.204 | |
| Gender, number of males (%) | 12 (63.5) | 8 (40) | 0.148 | |
| Premorbid MFAC (SD) | 6.8 (0.7) | 6.7 (0.9) | 0.813 | |
| Types of fracture (%) | 0.329 | |||
| Femoral neck | 10 (52.6) | 12 (60) | ||
| Inter-trochanteric | 7 (36.8) | 8 (40) | ||
| Sub-trochanteric | 2 (10.5) | 0 (0) | ||
| Types of operation (%) | 0.276 | |||
| Hemiarthroplasty | 7 (36.8) | 6 (30) | ||
| Total hip replacement | 0 (0) | 3 (15) | ||
| Dynamic hip screw | 2 (10.5) | 0 (0) | ||
| Cannulated screw | 2 (10.5) | 2 (10) | ||
| Intramedullary nail | 8 (42.1) | 9 (45) | ||
| Hospitalization (days), mean (SD) | 26.5 (3.9) | 26.5 (4) | 0.728 | |
| Caregiver relationships (%) | 0.418 | |||
| Spouse | 8 (42.1) | 5 (25) | ||
| Children | 11 (57.9) | 13 (65) | ||
| Relative | 0 (0) | 1 (5) | ||
| Domestic helper | 0 (0) | 1 (5) | ||
| MFAC (SD) | 5.5 (1) | 5.3 (1.1) | 0.550 | |
| EMS (SD) | 11.8 (5.2) | 12 (3.5) | 0.687 | |
| LEFS (SD) | 25.7 (15.9) | 20.5 (7.9) | 0.496 | |
| M-CSI (SD) | 6 (6.4) | 4.8 (4.7) | 0.879 | |
Primary outcomes
There was a significant increase in MFAC, EMS and LEFS in both groups from baseline to the second month, yet no significant difference between the groups was observed. The experimental group showed a significant increase in EMS and LEFS from baseline to the first month, whilst the control group showed a significant increase in LEFS only (Table 4). There were no significant differences in MFAC, EMS and LEFS among both groups at the first month and second month (Table 5).
| From baseline to one month (T0–T1) | Between-group | From baseline to two months (T0–T2) | Between-group | |||
|---|---|---|---|---|---|---|
| Exp. (n=19) | Con. (n=20) | p-value | Exp. (n=19) | Con. (n=20) | p-value | |
| MFAC | 0.901 | 0.728 | ||||
| Median | 1 | 0.5 | 1 | 1 | ||
| (IQR) | (0–1) | (0–1) | (0.5–2) | (0–1.5) | ||
| p-Value | 0.266 | 0.399 | 0.002∗ | 0.008∗ | ||
| EMS | 0.351 | 0.647 | ||||
| Median | 3 | 2 | 4 | 3 | ||
| (IQR) | (1–5.5) | (0.5–5) | (2–7) | (2.5–5) | ||
| p-Value | 0.004∗ | 0.081 | <0.001∗ | <0.001∗ | ||
| LEFS | 0.945 | 0.411 | ||||
| Median | 16 | 13.5 | 18 | 22 | ||
| (IQR) | (10.5–22) | (8.5–21) | (13–34) | (19–33) | ||
| p-Value | 0.005∗ | 0.01∗ | <0.001∗ | <0.001∗ | ||
| M-CSI | 0.184 | 0.531 | ||||
| Median | −1 | −2 | −2 | −3 | ||
| (IQR) | (−3–0) | (−4.5–−1) | (−7–0) | (−6–−1) | ||
| p-Value | 0.370 | 0.002∗ | <0.001∗ | <0.001∗ | ||
| Friedman test | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline (T0) | First month (T1) | Between-group | Second month (T2) | Between-group | p-value | ||||||
| Exp. (n=19) | Con. (n=20) | Exp. (n=19) | Con. (n=20) | p-value | Exp. (n=19) | Con. (n=20) | p-value | Exp. (n=19) | Con. (n=20) | ||
| MFAC (1–7) | 0.22 | 0.11 | <0.001∗ | 0.001∗ | |||||||
| Median | 6 | 5 | 6 | 6 | 6 | 6 | |||||
| (IQR) | (5–6) | (4.5–6) | (6–6) | (5–6) | (6–7) | (6–6) | |||||
| EMS (0–20) | 0.43 | 0.34 | <0.001∗ | <0.001∗ | |||||||
| Median | 14 | 13 15 | 15 | 17 | 17 | ||||||
| (IQR) | (8.5–15) | (10–14) | (14–17.5) | (14–16) | (15.5–19.5) | (16–18) | |||||
| LEFS (0–80) | 0.34 | 0.43 | <0.001∗ | <0.001∗ | |||||||
| Median | 20 | 20 | 42 | 34.5 | 52 | 47.5 | |||||
| (IQR) | (17.5–28) | (14–26) | (29.5–56) | (26–47.5) | (30–62.5) | (34.5–54) | |||||
| M-CSI (0–26) | 0.19 | 0.51 | <0.001∗ | <0.001∗ | |||||||
| Median | 4 | 3.5 | 1 | 0 | 0 | 0 | |||||
| (IQR) | (0–11.5) | (1–7) | (0–5) | (0–3) | (0–1.5) | (0–1.5) | |||||
| Adherence (0–100%) | 0.03∗ | 0.09 | |||||||||
| Median (%) | 100 | 75 | 95 | 67.5 | |||||||
| (IQR) (%) | (78.5–100) | (54–100) | (76.5–100) | (50–100) | |||||||
Secondary outcomes
The experimental group showed better exercise adherence than the control group with significant difference in the first month. Although exercise adherence in the experimental group was still higher than the control group in the second month, there was no significant difference among the two groups (Table 5). Significant reduction in M-CSI was observed in both groups from baseline to the second month, yet no significant difference between groups was observed (Table 4).
Discussion
The aim of this study was to investigate the efficacy of a home-based rehabilitation program using a mobile app on elderly patients with hip fracture and their caregivers. The results showed that these patients using the mobile app had better exercise adherence when compared to using pamphlets. There were two features in the mobile app, which pamphlets could not provide, that might lead to higher motivation of patients in performing exercises. First, a daily exercise reminder using text messages was delivered to patients’ mobile devices. This feature was highly noticeable as the reminder activated with an audible alarm that drew the attention of the elderly patients. The patients could then see the motivational messages as soon as they picked up the mobile devices. Text messaging was already shown to be an effective intervention in improving exercise adherence among elderly population.33 Second, video-guided exercise programs were embedded in the mobile app so that patients could perform exercise along with the videos. Compared to text and illustrations, video demonstrations were able to provide clear and timely instructions, such as close-up views and verbal cues for better exercise techniques. This mode of exercise instruction might improve patients’ confidence in performing the home-based exercises without therapists’ supervision. A study suggested that there was a positive correlation between self-efficacy and adherence rate to exercise interventions for hip fracture patients.34 The effect of increased exercise adherence in patients using the mobile app was not existent in the second month. It might be due to a possibility that the patients began to disregard the daily exercise reminder, as the effect of motivational messages was known to diminish over time.35 Future development of mobile app could investigate the possibility of sending feedback to the therapists when under-utilization of the mobile app was detected, so that they could arrange timely home visits for exercise re-enforcement.
Patients using either mobile app or exercise pamphlets had significant improvement in the primary outcomes (MFAC, EMS and LEFS) over two months, however, there were no additional benefits demonstrated in using the mobile app. It was thought that improvement in exercise adherence would lead to better physical performance. However, this relationship was not established in the study. A possible reason for this phenomenon might be that the exercises in the home-based rehabilitation program focused on strengthening and functional movements only, but the primary outcomes also take into account the performance in other aspects such as walking speed, stairs walking and outdoor activities. The outbreak of COVID-19 during the study period might have reduced patients’ motivation to participate in outdoor activities, thus limiting the potential in physical performance and self-efficacy. Furthermore, a follow-up period of two months might also not be sufficient to observe the effects of mobile apps on hip fracture patients. A study demonstrated that hip fracture patients could have physical improvements in a longer study period of six–nine months.24 Further studies could be done to investigate the benefits of the mobile app on physical performance and self-efficacy over a longer period of time.
In this study, caregivers from both groups reported relatively low stress level. It was different from the observation in other studies that caregivers experienced a moderate-to-high level of stress after the hip fracture patients got discharged from the hospital.11,36 It could be due to the fact that the participants in this study had a high baseline mobility status and did not require much assistance in transfer and ambulation at home. Hence, the provision of the mobile app for the experimental group or the educational pamphlet for the control group might not make a difference in reducing the stress of these caregivers. Further studies could be conducted to investigate the efficacy of the mobile app in reducing caregiver stress with dependent patients.
Caregiver support is key to ensure the successful implementation of home rehabilitation using the mobile app, especially for elderly patients who would have a higher chance to experience issues with modern technology. Several common technical issues were identified throughout the study. Many participants were unable to install the mobile app in their mobile devices alone, since they often forgot or did not have the record of username and password to authorize apps installation. Some participants thought that the mobile app could be installed in their mobile devices, however, they found that the operating system of the devices was neither iOS nor Android. The screen size of some participants’ mobile devices was found to be too small that videos and texts within the app became unreadable, and their caregivers had to provide these participants with another mobile device. A recommendation to resolve the above issues is to establish a checklist of mobile device requirements and involve caregivers early before hospital discharge, so as to prevent any delays in home rehabilitation.
There were several limitations in this study. It was carried out during the outbreak of COVID-19 and the recruitment of participants was affected. The small sample size reduced the power to detect differences between the groups. A longer follow-up period would help understand the long-term effect of a home-based rehabilitation program on geriatric hip fracture patients. Ascertainment bias might occur since neither outcome assessors nor participants were blinded from knowing which treatment group they belonged to. Participants and their caregivers were involved in this study, therefore, the results could not be generalized to elderly patients who live alone.
Conclusions
Use of the mobile app improved exercise adherence, yet it did not improve physical performance, self-efficacy and reduce caregiver stress when compared to a standard home rehabilitation program for elderly patients with hip fracture. Further studies to investigate the benefits of mobile apps are required.
Conflict of Interest
The authors declare no conflicts of interest relevant to this work.
Funding/Support
The authors received no financial support for the research, authorship and/or publication of this paper.
Author Contributions
Conception and design of the study were carried out by Kin Ming Ken Lau, Fuk On Titanic Lau, Mun Cheung Herman Lau and Sheung Wai Law. Acquisition of data was carried out by Kui Ching Cheng and Tin Sing Keith Lau. Analysis and interpretation of data were carried out by Kui Ching Cheng and Andy S. K. Cheng. Drafting of the manuscript was carried out by Kui Ching Cheng, Kin Ming Ken Lau, Andy S. K. Cheng and Tin Sing Keith Lau. Manuscript revision was carried out by Tin Sing Keith Lau, Fuk On Titanic Lau, Mun Cheung Herman Lau and Sheung Wai Law. All authors approved the final manuscript to be published.