The seventh cervical vertebra is an appropriate landmark for thoracic kyphosis measures using distance from the wall
Abstract
Background: Hyperkyphosis is frequently found nowadays due to the change in current lifestyles and age-related system decline. A simple hyperkyphosis measurement can be made easily using the perpendicular distance from the landmark to the wall. However, the existing evidence applied two different landmarks [occiput and the seventh cervical vertebra (C7)] and the measurement using rulers was susceptible to error due to their misalignment.
Objective: To assess an appropriate landmark for thoracic kyphosis measurement using distance from the wall (KMD), by comparing between occiput and C7, as measured using rulers and verified using data from a specially developed machine, the so-called infrared-gun kyphosis wall distance tool (IG-KypDisT), and the Cobb angles.
Methods: Community-dwelling individuals with a risk of thoracic hyperkyphosis (age ≥10≥10 years, n=43n=43) were cross-sectionally assessed for their thoracic hyperkyphosis using the perpendicular distance from the landmarks, occiput and C7, to the wall using rulers and IG-KypDisT. Then the Cobb angles of these participants were measured within seven days.
Results: The outcomes from both landmarks differed by approximately 0.8cm (p=p= 0.084). The outcomes derived from C7 were more reliable (ICCs>>0.93, p<p<0.001), with greater concurrent validity with the radiologic data (r=r= 0.738, p<p<0.001), with the overall variance predicted by the regression models for the Cobb angles being higher than that from the occiput (47–48% from C7 and 38–39% from occiput). The outcomes derived from rulers and IG-KypDisT showed no significant differences.
Conclusion: The present findings support the reliability and validity of KMD assessments at C7 using rulers as a simple standard measure of thoracic hyperkyphosis that can be used in various clinical, community, and research settings.
Introduction
Thoracic hyperkyphosis is a progressive condition with backward deviation of the thoracic spine and a Cobb angle exceeding 40∘.1 This condition can be found in those aged 10 years and over, approximately one-third of all teenagers and adults, and 40% of older adults.2,3 The change in current lifestyles whereby many people spend considerable time in an excessively flexed posture using computers and social media, combined with the reduction in physical activities, may hasten the development of hyperkyphotic spine in young people.2,3,4
The thoracic hyperkyphosis can introduce various adverse health consequences depending upon the severity of the condition, such as diminished self-confidence, musculoskeletal pain, impaired pulmonary and physical functions, elevated resting energy consumption, and increased risk of falls and vertebral fractures that further accelerate the progression of thoracic curvature and its negative consequences.5,6 Therefore, a standard practical measure plays crucial roles in the early detection and periodic follow-up of abnormality, and in promoting treatment effectiveness and minimizing the harmful consequences that may occur due to thoracic hyperkyphosis.7,8,9,10
Of all the existing hyperkyphosis measures, the occiput–wall distance (OWD) is a practical measure that can be executed easily using two rulers to measure the perpendicular distance from the landmark to the wall while standing against it.11,12 However, the OWD faces some criticisms, including the following: using the occiput as a landmark could confound data interpretation regarding thoracic hyperkyphosis and increase the chance of errors due to individuals moving their heads, having forward head posture, and the varying shapes of the skulls.10,13,14 Moreover, the data taken from two rulers were susceptible to errors due to their misalignment, e.g., not parallel to the landmark and not perpendicular to the wall. Furthermore, the outcomes in terms of distance could limit data comparison with other hyperkyphosis measures that are mostly reported in terms of spinal angles.11,12,14 Consequently, some recent studies have applied the bony prominence of the seventh cervical vertebra (C7) as a landmark for the measurement because it is a stable point over the superior limit of the thoracic spine.15,16 Nevertheless, there was no evidence to confirm the validity and reliability of the outcomes from both landmarks, particularly covering the ages of all of those at a risk of thoracic hyperkyphosis (10 years old and over). Therefore, this study investigated the intra- and inter-rater reliabilities and concurrent validity of kyphosis measurement using distance from the wall (KMD) when measured using rulers at the occiput and C7 and verified using data from a specially developed machine, the so-called infrared-gun kyphosis wall distance tool (IG-KypDisT), and the radiologic data (Cobb’s method). In addition, the study explored a predictive equation for the overall variance, including KMD from each landmark, from the regression models to determine the Cobb angles. The findings would provide clear evidence to confirm an appropriate landmark for KMD using rulers for screening and monitoring thoracic hyperkyphosis in various clinical, community, and research settings, especially in this COVID-19 pandemic period with limited access to people in a hospital.
Methods
Participants
Community-dwelling participants with or without signs or symptoms associated with thoracic structural hyperkyphosis, i.e., those who are unable to consciously straighten the spinal column,3 were recruited by directly contacting the community leaders. The inclusion criteria were as follows: age ≥10≥10 years, body mass index << 29.9kg/m2, and OWD ≥≥ 6.5cm while attempting to straighten the spinal column when measured using rulers by an experienced assessor.12,17 The exclusion criteria included any signs and symptoms that might affect participation in this study and confound data interpretation, i.e., having abnormal fat mass in the upper back or winged scapula that could increase the distance from the wall when standing against it, and scoliosis as determined using Adam’s test. Additional exclusion criteria were any conditions with contraindications for X-ray examination (i.e., pregnancy or cancer),18 difficulty in maintaining a standing posture, and inability to understand and follow a command used in the study. The sample size calculation for a primary objective (concurrent validity) using the correlation coefficient (rr) from a pilot study (n=20n=20, r=r=0.42), with the significance level set at 0.05 and the power level set at 0.8, indicated that the study required at least 42 participants. Previous studies relating to the reliability of kyphosis measurements applied at least 15 participants.8,15,18,19 Participants provided a written informed consent that was approved by the Institutional Ethics Committees for Human Research (HE592270) prior to participation in this study.
Research protocols
The eligible participants were involved twice in this observational study within seven days. At the first time, they were interviewed for their demographics and assessed for their severity of thoracic hyperkyphosis using KMD. Within the following seven days, participants were informed to arrive at the hospital to complete a lateral spinal radiographic examination (Cobb’s method). Details of the measurements were as follows.
Kyphosis measured using the distance from the wall
It has been reported that the KMD data measured with the rulers were susceptible to errors due to their misalignment.10,11,14 Thus, the KMD data measured with rulers in this study were verified using IG-KypDisT [Patent Application No. 1701004049; Fig. 1(a)]10 that was specially developed to ensure perpendicular distance from the landmarks to the wall using two-plane gyroscopes (up to 1mm). Outcomes of the tool showed excellent correlation to the Cobb angles (r=r= 0.92, p<p<0.001).11 Therefore, IG-KypDisT was used to verify the KMD derived from rulers. Details of the measurements were as follows.
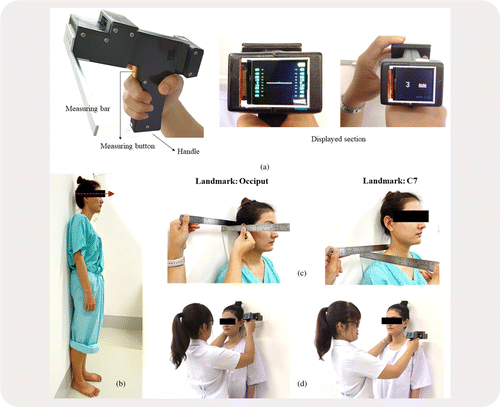
Fig. 1. Kyphosis measurements using the distance from the wall: (a) IG-KypDisT and its components. (b) Starting position for KMD. (c) KMD using rulers. (d) KMD using IG-KypDisT.
Starting position. Participants stood upright with bare feet — as tall as possible — with their heels, sacrum, and back against the wall, and with the head in a neutral position as determined using the inferior orbital margin and the superior margin of the acoustic meatus in a horizontal plane [Fig. 1(b)].1,11,12,15
Methods of measurement. We used the following methods of measurement:
(1) Rulers: Two rulers were used to quantify the outcomes of each landmark (occiput or C7). The first ruler was placed on the landmark and another ruler was used to measure the perpendicular distance from the landmark to the wall [Fig. 1(c)].
(2) IG-KypDisT: Prior to the measurement, IG-KypDisT was calibrated with a flat upright surface. Then, an experienced rater placed the measuring bar of IG-KypDisT in contact with the landmark [Fig. 1(d)] and adjusted the tool perpendicularly with the wall until they noticed a white line on the monitor in a horizontal plane [Fig. 1(a)]. Then the rater pressed the measuring button to obtain the outcomes.
The sequences of measurement using rulers and IG-KypDisT were randomly ordered, and the average findings over 3 trials/landmark were used for data analysis.
Reliability study
Raters were three physiotherapists who had clinical experience ranging from 2 years to 9 years. Prior to the measurement, the raters were trained for a standard KMD protocol, including the starting position, instructions, and measurement methods, for approximately 20 min. Then they practiced the measurements on four non-participants. Subsequently, the raters measured the KMD at the occiput and C7 using rulers on participants who agreed to be involved in the reliability study for 3 trials/landmark. The outcomes over the three trials of each rater from each landmark were used to analyze the intra-rater reliability, and the average data over the three trials of all raters were used to report the inter-rater reliability.15,19
Kyphosis measured using the Cobb’s method
All participants were filmed covering the area from the first to the 12th thoracic vertebra (T1–T12). Participants stood upright with their shoulders and elbows flexed at 90∘ to prevent the thoracic curvature from overlapping with the upper limbs.12,18 Then, the radiologic image was uploaded for calculation of the Cobb angles by an experienced rater using the Surgimap Spine v1.2 software (Nemaris, Inc., New York, NY, USA).19,20 The rater drew the first line along the upper surface of the fourth thoracic (T4) vertebral end-plate, and the second line along the lower surface of the 12th (T12) vertebral end-plate. Then the software automatically generated the Cobb angles based on the intersection of the two lines.12,19,20 The method was repeated for three trials, and the average angle was used for data analysis.
Statistical analysis
The Kolmogorov–Smirnov test was applied to assess the normality of the data distribution. Descriptive statistics were used to explain the demographics and findings of the study. With normal data distribution, the Bland–Altman plots and dependent samples tt-test were used to indicate the outcome differences between the rulers and IG-KypDisT for each landmark. The Pearson correlation coefficient was then applied to quantify the levels of correlation between the KMD data at each landmark and the Cobb angles. The levels of correlation coefficient were interpreted as negligible (below 0.30), low (0.30–0.50), moderate (0.50–0.70), and high (above 0.70).21,22 Then, the stepwise multiple linear regression analysis was utilized to formulate a predictive equation from all possible demographic and KMD variables relating to the presence of thoracic kyphosis (i.e., age, gender, bodyweight, height, and KMD) to determine the Cobb angles.3 Adjusted R2R2 was used to indicate the most appropriate equation, with an R2R2 value of 1 indicating that the data perfectly fit the linear model.23 The intra-class correlation coefficients (ICCs),3 i.e., participants were assessed by raters who were only the raters of interest, were used to quantify the reliability of KMD outcomes at each landmark. The reliability was considered as poor (below 0.50), moderate (0.50–0.75), and high (above 0.75).20,21 Moreover, the absolute reliability of the KMD at each landmark was further assessed and reported in terms of the standard error of measurement (SEM), using the equation SD ××√1−ICCs√1−ICCs, and the minimal detectable change (MDC), using the equation SEM ×1.96×√2×1.96×√2.15 The p<p< 0.05 indicated significant differences.
Results
Forty-three participants completed the validity study (average Cobb angle = 40.5∘, ranging from 11.3∘ to 67.7∘), and 17 participants were also involved in the reliability study (average Cobb angle = 35∘, with a range of 28.1– 42∘) (see Table 1 and Supplementary Material). Most participants did not have any signs and symptoms of thoracic hyperkyphosis, except for two older participants who had vertebral fractures (radiologic data).
| Validity study | Reliability study | |
|---|---|---|
| Variable | (n=43n=43) | (n=17n=17) |
| Age† (years) | 52.8±± 25.2 | 48.8±± 22.1 |
| (45–60.5) | (37.4–60.2) | |
| Body mass index† (kg/m2) | 23.5±± 3.5 | 22.6±± 2.9 |
| (22.4–24.6) | (21.2–24.1) | |
| Cobb angles† (deg) | 40.5±± 13.3 | 35±± 13.5 |
| (36.5–44.6) | (28.1–42) | |
| Gender: female: number (%) | 21 (48) | 7 (41) |
Validity of KMD when measured at occiput and C7
The KMD outcomes at each landmark showed no significant differences between the tools (p>p>0.05). However, the KMD outcomes from rulers and IG-KypDisT measured at the occiput showed a wider range of differences than those at C7 (Fig. 2). In addition, the KMD outcomes measured at C7 were longer than those at the occiput by approximately 0.8cm (8.5 ±± 1.8cm and 9.3 ±± 2.7cm, p=p=0.084). Furthermore, the KMD outcomes measured using rulers at C7 showed significant correlation with the data from IG-KypDisT (r=r= 0.872, p<p<0.001) and Cobb angles (r=r= 0.738, p<p<0.001), and were higher than those derived at the occiput (r=r= 0.636 with IG-KypDisT and r=r= 0.442 with Cobb angle, p<p<0.003, Fig. 2). Among all possible predictive variables, only age and KMD data were significant for determining the Cobb angles (p<p<0.001), whereby the overall variance predicted by the regression models when measured at C7 (47–48%, Table 2) was higher than that derived at the occiput (38–39%, Table 2).
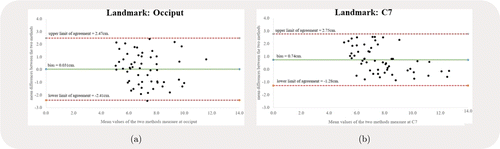
Fig. 2. Bland–Altman plots for kyphosis measurement using distance from the wall.
| Landmark | Tool | Predictive equation* | Adjusted R2R2 |
|---|---|---|---|
| Occiput | Rulers | 2.06(KMD)+0.26(age)+9.44 | 0.39 |
| IG-KypDisT | 1.48(KMD)+0.24(age)+15.44 | 0.38 | |
| C7 | Rulers | 2.49(KMD)+0.13(age)+10.43 | 0.47 |
| IG-KypDisT | 2.11(KMD)+0.15(age)+14.13 | 0.48 |
Reliability of KMD when measured using rulers at the occiput and C7
The KMD data measured using rulers showed no significant differences among the three raters, with excellent intra- and inter-rater reliabilities and small SEM and MDC, particularly when measured at C7 (ICCs≥≥0.933, p<p<0.001, Table 3).
| Landmark | Variable | Rater 1 | Rater 2 | Rater 3 | pp-Value |
|---|---|---|---|---|---|
| Occiput | Distance† (cm) | 8.16±± 1.48 | 7.45±± 1.07 | 8.06±± 1.82 | 0.337‡ |
| Intra-rater reliability (95% CI) | 0.995 | 0.995 | 0.999 | <<0.001* | |
| (0.989–0.998) | (0.988–0.998) | (0.997–0.999) | |||
| SEM/MDC (cm) | 0.10/0.29 | 0.08/0.21 | 0.06/0.16 | ||
| Inter-rater reliability (95% CI) | 0.811 (0.576–0.926) | <<0.001* | |||
| SEM/MDC (cm) | 0.65/1.80 | ||||
| C7 | Distance†(cm) | 8.32±± 1.40 | 8.36±±1.83 | 8.64±± 1.74 | 0.839‡ |
| Intra-rater reliability (95% CI) | 0.994 | 0.996 | 0.998 | <<0.001* | |
| (0.986–0.998) | (0.992–0.999) | (0.995–0.999) | |||
| SEM/MDC (cm) | 0.11/0.30 | 0.12/0.32 | 0.08/0.22 | ||
| Inter-rater reliability (95% CI) | 0.933 (0.850–0.974) | <<0.001* | |||
| SEM/MDC (cm) | 0.42/1.18 |
Discussion
This study sought to identify a more valid and reliable landmark, C7 or occiput, in determining KMD as a simple standard clinical screening measure of individuals at risk of structural thoracic hyperkyphosis. The findings suggest that, after proper training, the KMD measured at C7 using two rulers is more valid and reliable than that derived from the occiput when verified using the data from IG-KypDisT and Cobb angles (Fig. 2, Tables 2 and 3).
The wider range of differences in KMD outcomes from rulers and IG-KypDisT when measured at the occiput as compared to those at C7 (Fig. 2) reflect the characteristics of both landmarks. The KMD measurement at the occiput could increase the chance of errors due to the participants moving their heads,13,14,15 hair thickness, and varying shapes of the skulls.1,11 Martinez-Abadias24 explored the phenotypic and genetic patterns of human skulls, and found substantial genetic variations in human skull sizes and shapes. In contrast, the bony prominence of C7 is a stable point over the superior limit of the thoracic spine.11,15,16 Therefore, the KMD outcomes when measured at C7 using rulers were similar to those from IG-KypDisT (Fig. 2).
The slight differences of KMD data between the occiput and C7 reflect normal body structure when considered in a sagittal plane. The bony prominence of C7 was closer to the body midline, and thus farther from the wall than the occiput when standing against the wall. Thus, the KMD data from C7 was longer than that at the occiput by approximately 0.8cm (p=p= 0.084), which was greater than the SEM or errors due to the measurements, from all raters (0.06–0.42, Table 3). The findings implied the true difference when measuring the KMD using different landmarks, i.e., the occiput or C7, and suggested using the same landmark for data comparisons over trials for the KMD.
The significant correlation between KMD and Cobb angles may reflect the effects of spinal kinematic linkage. The change of spinal curvature in a particular area influences the change of other spinal areas to compensate and improve balance of the spinal column.14 Therefore, increased thoracic curvature could increase cervical lordosis that subsequently enhanced the perpendicular distance from C7 or occiput to the wall. Nevertheless, the variation of KMD outcomes when using occiput as a landmark could confound the validity and predictive ability for thoracic angles. Therefore, the validity and overall variance predicted of the KMD measured at C7 by the regression model were found to be better than those of the occiput (Tables 2 and 3). Therefore, after proper training, the KMD at C7 using rulers could be used as a standard simple and practical measure for screening and data transferring among the various clinical, community, home-based, and research settings.
Nonetheless, the levels of correlation of KMD and Cobb angles in this study were lower than those reported previously (r=r= 0.902, p<p<0.001 compared to Flexicurve).15 These differences may be associated with the (1) age of the participants, (2) standard method used to verify the outcomes, and (3) starting position of the measurements. The concurrent validity of KMD was previously assessed in participants who were aged 60 years and over using Flexicurve, an indirect standard kyphosis measure.10,15 Older adults have rather fixed spinal columns that result in structural hyperkyphosis and reliable outcomes over trials even when changing the postures, or lifting the arms upward for Cobb’s measurements. However, indirect measurements using Flexicurve are susceptible to errors due to palpation skill for a proper bony landmark (i.e., spinous processes of T12) and the changes in the shape of Flexicurve once it is removed from the spine.15 On the contrary, this study recruited participants aged 10 years and over to capture those at a risk of thoracic hyperkyphosis due particularly to the change in the current life styles, age-related postural changes and system decline, including those aged 11–14 years (30%), 15–18 years (22%), 20–50 years (38%), and >60>60 years (22–44%).1,2,3 Being younger individuals with an average age of 50.5±± 26 years (ranging from 11 years to 88 years, Table 1), some participants might have a relatively flexible spine. Although the researchers attempted to recruit participants who were unable to consciously straighten the spinal column, i.e., having structural hyperkyphosis,3 some teenager participants might be unable to straighten their spinal columns due to muscle weakness. However, the radiologic assessments with lifting the arms forward through 90∘ may alter their thoracic kyphosis and affect the levels of correlation found in this study. This assumption is associated with a previous study that recruited participants aged 18 years and above (average age 54.5 ±± 17.5 years) and also found similar correlation as that reported in this study (r=r= 0.72).25
Limitations
Our findings provide strong evidence to support the use of C7 as an appropriate landmark for KMD using rulers. However, there are some limitations of the findings. First, this study recruited totally 43 participants covering all those with a risk of hyperkyphosis (aged 10 years and over). However, with the COVID-19 crisis, the researchers were unable to recruit the participants according to the proportion reported in previous studies, aged 11–14 years (30%), 15–18 years (22%), 20–50 years (38%), and >60>60 years (22–44%).1,2,3 Moreover, time of the day for the measurements might affect the findings of the study. Therefore, all participants were measured for KMD using rulers and IG-KypDisT altogether in a single visit. However, the radiologic assessments were scheduled according to hospital appointments within the following seven days. The variation in the assessment schedules could influence the correlation found between KMD and the Cobb angles. Furthermore, the overall variance predicted by the regression model of KMD for the Cobb angles might be influenced by other factors, such as the apex of hyperkyphosis, bone morphology, and system functions. The assessments of these variables need further invasive methods and other mobility tests that would increase the complexity and are not in line with the original aim of a simple measure of KMD. Therefore, a further study may recruit the participants according to proportion reported previously to promote generalizability of the findings.
Conclusions
The KMD is a simple and practical measure for thoracic hyperkyphosis. However, the existing evidence applied two different landmarks and the measurement using rulers was susceptible to errors due to their misalignment. Our findings support the reliability and validity of KMD assessments at C7 using rulers as a simple and practical measure of thoracic hyperkyphosis that can be used in various settings, such as hospitals, clinics, schools, offices, or research laboratories.
Conflict of Interest
The authors have no conflicts of interest relevant to this paper.
Funding/Support
This work was supported by the Grant for Post-Doctoral Training Program from Khon Kaen University (grant no. PD2665-04).
Author Contributions
All authors were responsible for the research conceptualization, study design, and final approval of the manuscript. Arpassanan Wiyanad, Patcharawan Suwannarat and Pakwipa Chokphukiao were also involved in data collection. Arpassanan Wiyanad also took part in statistical analysis, data interpretation, and drafting of the manuscript. Pipatana Amatachaya and Thanat Sooknuan were additionally responsible for IG-KypDisT developments and calibration. Sugalya Amatachaya was also responsible for research management, funding application, data interpretation, and finalization of the manuscript.
Acknowledgments
The researchers sincerely thank Mr. Patiphan Tochang and Ms. Kanjana Kramkrathok for their kind support in the equipment used in the study.