Feasibility and utility of intraoperative optical coherence tomography during vitreoretinal surgery: A 4-year report in Chinese population
Abstract
Purpose: To introduce the application of intraoperative optical coherence tomography (iOCT) in pars plana vitrectomy (PPV) for various vitreoretinal diseases, and to report the 4-year assessment of feasibility and utility in Chinese population. Methods: Retrospective case series of patients who underwent PPV and iOCT scan at Eye Hospital of Wenzhou Medical College from January 2016 to January 2020. Clinical characteristics were documented before operation, and we intraoperatively recorded the time and results of iOCT scanning, specific surgical maneuvers performed, the consistency with the planned strategies before surgery, the type of OCT images obtained, and adverse events (AEs). The surgeon feedback was collected to evaluate the utility of iOCT during surgery. Results: In total 339 eyes successfully completed iOCT scan, with an average scanning time of 3.54±2.33.54±2.3min, including 59 cases of idiopathic macular hole (iMH), 134 cases of idiopathic epiretinal membrane (iERM), 33 cases of lamellar macular hole (LMH), 40 cases of high myopic maculopathy, 13 cases of vitreous macular traction (VMT), 60 cases of dense vitreous hemorrhage (VH). The iOCT findings were not consistent with examination under the operating microscope in 49 cases (14.5%), including 29 cases (8.6%) which changed the operation strategies during surgery. The Hole-door phenomenon arose in 20 cases (33.9%) of iMH and 3 cases (25%) of high myopic MH after ILMs peeling. Moreover, the residue ERM was observed in nine cases (6.7%) of iERM and two cases (14.3%) in high myopic ERM after ILMs peeling. Some new surgical methods could also be confirmed using iOCT. Conclusion: The application of iOCT has a significant clinical functionality in vitreoretinal surgery, providing the surgeon with a new surgical understanding, guiding the selection of a more reasonable operative procedure during surgery, predicting postoperative recovery and improving postoperative outcomes.
1. Introduction
Recently, as a vital auxiliary tool for clinical diagnosis and treatment of ophthalmic diseases, optical coherence tomography (OCT) contributes to diagnosis, conducts therapeutic monitoring, and enhances clinical decision-making in numerous ophthalmic conditions.1 Considering that OCT has the advantage of intuitive display, many scholars consider that it can be applied to the operation process to obtain a real-time observation of the intraoperative status, and to assist the surgeon in the operation. Though still an emerging technology, numerous studies and reports have described the utility and value of this technology as it applies to ophthalmic surgery.
Intraoperative optical coherence tomography (iOCT) is a new type of OCT that improves on the platform of traditional OCT to meet the requirements of patients with vitreoretinal surgery in supine position for real-time OCT inspection during surgery.2,3 The surgeon can use the iOCT technology to intuitively observe the changes of the macular morphology during the operation, and choose a more suitable surgical method in time. The previous research of the research team also proved this value.2,3,4,5,6,7,8,9,10 As the development of modern imaging technology, iOCT has experienced three generations of development, and the scanning technology and carrying platform have been continuously improved. The latest integrated microscope iOCT can perform real-time scanning.11,12,13 While at present, there is a lack of widespread use of microscope-integrated iOCT in China, and there are few reports on iOCT. Therefore, our research team has performed iOCT examinations on the eyes by undergoing vitreoretinal surgery in our hospital within four years. The results of its application are reported as follows.
2. Materials and Methods
2.1. Study design
This is a retrospective study of consecutive patients undergoing pars plana vitrectomy (PPV) and iOCT scanning at Eye Hospital of Wenzhou Medical College from January 2016 to January 2020. The study adhered to the Declarations of Helsinki and the institutional guidelines. Informed written consent was obtained from all the patients.
2.2. Patient selection
All patients undergoing PPV and iOCT scanning were included in the study. The inclusion criteria for eyes included in this study were: with dense vitreous hemorrhage (VH) who cannot obtain OCT images two months before PPV, with idiopathic macular epiretinal membrane (iERM) or idiopathic macular hole (iMH), with LMH, with high myopic maculopathy, with vitreomacular traction (VMT). Exclusion criteria included eyes with the history of vitreoretinal surgery, and a severe turbidity of the refractive media, such as corneal leukoplakia or severe opacification of the posterior lens capsule.
2.3. Preoperative preparation
All patients routinely completed best corrected visual acuity (BCVA), intraocular pressure, IOL-Master (IOL-Master-700, Carl Zeiss Meditec AG, Jena, Germany), slit lamp microscope examination, fundus examination, OCT scanning (Spectralis OCT, Heidelberg, Germany) before operation, and preoperative BCVA was recorded as logMAR vision (light perception=logMARperception=logMAR 2.6, hand move=logMARmove=logMAR 2.3, finger count=logMARcount=logMAR 1.85.14 Axial length ≥26≥26mm and/or spherical refractive error>−6.00error>−6.00 diopters was recognized as highly myopic eyes. All patients signed an informed consent form before surgery. The intervention methods in this study followed the Declaration of Helsinki.
2.4. Surgical technique and iOCT scanning method
All the eyes underwent conventional 23-gauge or 25-gauge PPV. Eyes with VH and macular diseases separately underwent iOCT examination after removing the hemorrhage and completing all peeling membranes operations. The operation was performed by the same doctor. Adoptivue OCT (Optovue Company, USA, 2018.0.0.38; Fig. 1) was used with a scan speed of 26,000times/s using a wavelength of 830nm. The axial and lateral resolution was 5μμm and 11.4μμm, respectively. The iOCT scans were performed in 3D mode and crossline two scan modes. iOCT examinations were performed by the same ophthalmologist who has extensive experience in desktop OCT operations. During the examination, a sterile surgical patch was attached to the OCT lens. The patient maintained the surgical position (supine position), then the bottom wheels were moved to align the pupil area, then the focus was automatically adjusted to the retina plane and images were captured subsequently. During the whole procedure, the balanced salt solution was used to keep the cornea moist.
Fig. 1. The vehicle-mounted iOCT used in this study.
Data collected included the time and results of iOCT scanning, specific surgical maneuvers performed, the consistency with the planned strategies before surgery, type of OCT images obtained, and adverse events (AEs). The ophthalmologist also collected the surgeon feedback immediately following surgery for all cases, focusing on several specific areas of interest related to the microscope-integrated system and surgical procedure. This included value of iOCT to the procedure and specific impact on surgical decision-making based on surgeon’s perspective.
2.5. Statistical analysis
Statistical analysis was performed using SPSS 22.0 for Windows (SPSS, Inc, Chicago, IL). The visual acuity was presented with LogMAR throughout the whole study, and the descriptive analysis was used for all the ocular parameters discussed in this study. The baseline data such as patient age, axial length, and preoperative BCVA conformed to the normal distribution and were expressed as mean±standardmean±standard deviation.
3. Results
A total of 390 eyes were enrolled and 339 cases successfully completed the iOCT scan (86.9%), with an average scan time of 3.54±2.33.54±2.3min. The main reasons for the scan failure were high myopia or intraoperative corneal edema.
In this study, 339 patients who successfully completed iOCT scan, including 59 cases of iMH, 134 cases of iERM, 33 cases of LMH, 40 cases of high myopic maculopathy, 13 cases of VMT, 60 cases of dense VH. All results were summarized in Table 1.
| iMH n=59n=59 | iERM n=134n=134 | Dense VH n=60n=60 | LMH n=33n=33 | VMT n=13n=13 | High myopic maculopathy n=40n=40 | Total n=339n=339 | |
|---|---|---|---|---|---|---|---|
| Gender (male/female) | 13/46 | 48/86 | 28/32 | 8/25 | 5/8 | 12/28 | 114/225 |
| Age, year | 58.17±12.3958.17±12.39 | 66.13±8.4166.13±8.41 | 57.73±12.8757.73±12.87 | 66.13±9.0866.13±9.08 | 58.23±12.0858.23±12.08 | 59.43±11.6359.43±11.63 | 62.96±10.5662.96±10.56 |
| Axial length (mm) | 23.30±1.0523.30±1.05 | 23.44±1.1823.44±1.18 | 23.24±1.0423.24±1.04 | 23.05±1.0523.05±1.05 | 24.12±1.3024.12±1.30 | 29.04±1.8729.04±1.87 | 24.21±2.3624.21±2.36 |
| Preoperative BCVA (logMAR) | 1.34±0.521.34±0.52 | 0.55±0.410.55±0.41 | 1.53±0.521.53±0.52 | 0.40±0.290.40±0.29 | 0.55±0.310.55±0.31 | 0.70±0.520.70±0.52 | — |
| Postoperative BCVA at final follow-up (logMAR) | 0.50±0.320.50±0.32 | 0.31±0.250.31±0.25 | 0.55±0.410.55±0.41 | 0.22±0.150.22±0.15 | 0.30±0.130.30±0.13 | 0.35±0.330.35±0.33 | — |
| P | <0.01<0.01 | <0.01<0.01 | <0.01<0.01 | <0.01<0.01 | <0.01<0.01 | <0.01<0.01 | — |
Among 339 eyes, 49 cases (14.5%) were inconsistent with the results of iOCT examination and the observation under the operating microscope of the surgeon. Among them, the surgical strategies of 29 cases (8.6%) were changed during the operation and a more reasonable surgical method was selected, respectively, including an additional membrane-peeling surgery or the change of vitreous cavity tamponade. No complications such as endophthalmitis related to the examination occurred after the operation.
3.1. iOCT results of idiopathic macular hole(iMH)
A total of 59 cases of iMH undergoing iOCT scan were enrolled in this study. Of these eyes, 51 cases underwent conventional ILM peeling, 5 cases underwent ILM peeling with inverted flap technique, and the technique of peeled ILM reposition was applied in 3 cases.
According to the results of iOCT of 51 cases that underwent conventional ILM peeling, the images showed that the top areas of the MHs were all reduced, moreover, the inner retina bridge connection generated after peeling ILMs in 2 cases and the vitreous cavity tamponade was finally switched to air tamponade (Fig. 2), and a slim strip with high reflection arose on the edge of MH after peeling ILMs in 20 cases (33.9%), which was recognized as the Hole-door phenomenon (Fig. 3). In the five cases that underwent ILM peeling with inverted flap technique, the inverted ILM flap could be clarified using iOCT scan during the operation (Fig. 4), furthermore, the reposited ILM could also be confirmed in the iOCT images in the 3 cases who adopted the technique of peeled ILM reposition.
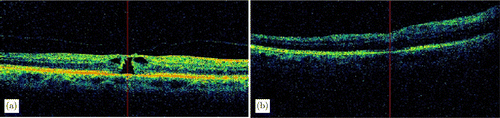
Fig. 2. (a) A preoperative OCT of an iMH patient. (b) The iOCT image revealed the occurrence of bridge connection of inner layers after the ILM peeling.
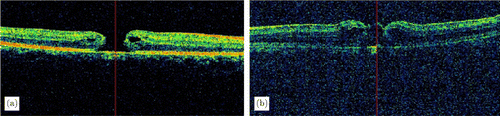
Fig. 3. (a) A preoperative OCT of a MH patient. (b) The iOCT image revealed the occurrence of slim stripes on the edge of MH after the ILM peeling.
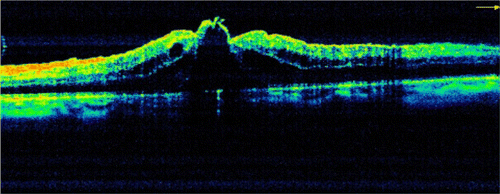
Fig. 4. A case underwent ILM peeling with inverted flap technique, the inverted ILM flap could be clarified using iOCT scan during the operation.
3.2. iOCT results of idiopathic epiretinal membrane(iERM)
A total of 134 cases of iERM undergoing iOCT scan were enrolled in this study. The aim of iOCT scan was mainly to observe the residual ERM and the secondary changes after peeling ERM.
The iOCT scan results showed that the residue ERM could be observed in 9 cases (6.7%), and an ERM re-peeling was conducted respectively in 4 cases, while the other 5 cases remained untreated since the residual ERM was too close to papilomacular fibers. Moreover, secondary changes after peeling ERM were detected in 74 cases (55.2%), including preretinal hemorrhage, inner retinal elevation, loss of nerve fiber layer, LMH and so on (Fig. 5).
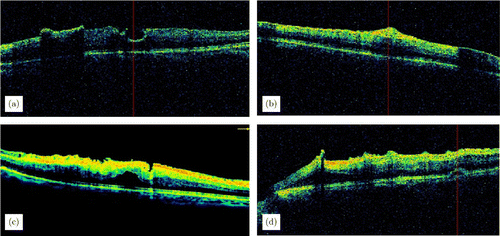
Fig. 5. (a) A case of epiretinal membrane residue after membrane peeling. (b) A case of nerve fiber layer elevation after membrane peeling. (c) A case of nerve fiber layer damage after membrane peeling. (d) A case of local neuroretina elevation after membrane peeling.
3.3. iOCT results of dense vitreous hemorrhage (VH)
A total of 60 cases of dense VH undergoing iOCT scan were enrolled in this study. The causes of dense VH in this study included diabetic retinopathy (43 cases), retinal vein occlusion (10 cases), and polypoidal choroidal vasculopathy (7 cases).
The iOCT examination was performed after removing the hemorrhage during the operation. According to the iOCT images, the normal macular structure was confirmed in 22 cases (36.7%), while each of the other 38 cases (63.3%) had macular abnormalities, and the main manifestations were macular edema (ME), macular epiretinal membrane (MER), LMH, macular atrophy, and so on. There were 16 cases (26.7%) whose iOCT results were not consistent with operator’s judgment under the microscope, including the MER which could not be observed by naked eyes under the microscope in 10 cases, mild ME in three cases, and the other three cases were diagnosed as ME under the microscope, while the iOCT images revealed the structure of macular area were normal. Based on the results of iOCT scan, an MER or ILM peeling was added in 13 cases (21.6%). All of the 10 cases of MER observed under iOCT scan received an additional ERM peeling and there was no recurrence in the follow-up (Fig. 6).
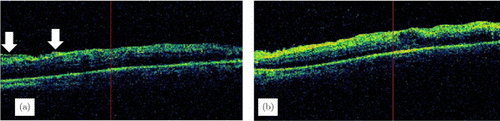
Fig. 6. (a) The iOCT image showed an epiretinal membrane (ERM) after the removal of VH. (b) The iOCT image showed that no epiretinal membrane residue after the peeling of ERM. White arrow: epiretinal membrane
3.4. iOCT results of high myopic maculopathy
The iOCT scan was completed in totally 40 cases of high myopic maculopathy, including 5 cases of macular foveoschisis (MF), 14 cases of epiretinal membrane (ERM), 5 cases of LMH, 12 cases of macular hole (MH), and 4 cases of VMT.
The iOCT results showed that the Hole-door phenomenon was observed in 3 cases (25%) with MH (Fig. 7), and the residue MER was detected in 2 cases (14.3%) with MER. Furthermore, after peeling the ERM or ILM, secondary changes were detected in 10 cases (25%), including preretinal hemorrhage and nerve fiber layer elevation. No full-thickness macular hole was observed in the eyes of MF after ILM peeling, however, one of the eyes was identified as a full-thickness macular hole under iOCT. In the 3 cases that underwent ILM peeling with inverted flap technique, the inverted ILM flap could be clarified using iOCT scan during the operation, furthermore, the reposited ILM could also be confirmed in the iOCT images in the 2 cases who adopted the technique of peeled ILM reposition.
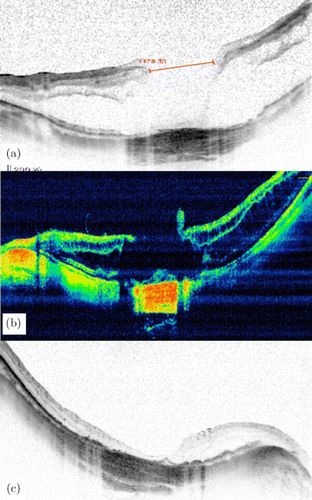
Fig. 7. The OCT images of patient diagnosed MH with high myopia. (a) Preoperative OCT showed a full-thickness MH combined with retinoschisis, the MH diameter was 1178μμm; (b) The iOCT image showed a moderately reflective band at the edge of the MH and (c) Postoperative OCT showed the MH was closed at one month after surgery.
3.5. iOCT results of other vitreoretinal diseases
A total of 33 cases of LMH undergoing iOCT scan were enrolled in this study. All patients adopted the conventional ILM peeling, there were no cases of secondary full-thickness hole after ILM peeling under iOCT examination, while secondary changes after peeling ILM were detected in 20 cases (60.6%), including preretinal hemorrhage and nerve fiber layer elevation.
A total of 13 cases of VMT undergoing iOCT scan were enrolled in this study, including 5 eyes of 5 males and 8 eyes of 8 females. The average age was 58.23±12.0858.23±12.08 years, and the average axial length was 24.12±1.3024.12±1.30mm, the average preoperative BCVA was 0.55±0.310.55±0.31. The results showed that vitreous traction was completely released after PPV, and no secondary change occurred.
4. Discussion
The clinical value of iOCT applied to vitreoretinal surgery lies in the detection of undetectable changes in the vitreous-retinal interface of the macular area through intraoperative scanning, which improves the operator’s understanding of the anatomic configuration and guides the surgical decision-making. As previously reported, iOCT examination was mainly used in macular disease to observe the morphological changes of the macular area after peeling ERM and ILM, and to guide subsequent surgical operations.10,15,16,17 The results of the DISCOVER study, a multi-center prospective study with the largest sample, showed that 29.2% of vitreoretinal surgeries have changed the surgeon’s surgical decision through the application of iOCT.1 The results of the application of iOCT in vitreoretinal surgery for four years in this study showed that the inconsistency rate between iOCT examination results and the operator’s microscope judgment reached to 14.5%, and 8.6% of the cases had changed the surgical method, indicating that iOCT has valuable clinical guiding significance for vitreoretinal surgery. Furthermore, no complications such as endophthalmitis related to the examination occurred after the operation.
iOCT is widely used in the surgery of macular disease, aiming to observe the extent of ERM and ILM peeling, the residual membranes, the secondary changes in ERM surgery, and to observe the morphological changes of the MH after ILM peeling. However, there are few researches on the correlation analysis between the intraoperative changes and postoperative changes in the iOCT examination of macular diseases. The results of this study showed that the inner retina bridge connection generated after peeling ILMs in some cases of iMH, thus a more reasonable surgical method was selected. Meanwhile, the results of iOCT analysis showed that a vertical slim strip with high reflection arose on the edge of MH after ILM peeling in 33.9% of cases, as previously reported, was recognized as the Hole-door phenomenon.18 In our previous research, for MHs with a diameter larger than 400μμm, the appearance of this phenomenon indicated a better prognosis, and it may be used as a scaffold to promote the closure of MH and the recovery of the outer photoreceptor cell layer.19 Second, the results of iOCT scan showed that the residue ERM could be observed in 9 cases of iERM, and an ERM re-peeling was conducted respectively in 4 cases. The incidence of secondary changes after membrane peeling reached 55.2%, mainly including preretinal hemorrhage, inner retinal elevation, loss of nerve fiber layer, lamellar macular hole, and so on. Moreover, compared with preoperative BCVA in this study, postoperative BCVA at final follow-up was significantly improved. Therefore, similar to the previous researches, the results of our study indicate that the application of iOCT has important reference value for whether to peel the membrane again during surgery and the recovery of visual function after surgery.20,21
Diabetic retinopathy and retinal vein occlusion are the most common causes of VH. As preoperative OCT examination in patients with dense VH cannot determine whether there were structural abnormalities in the macular area, according to the iOCT images, macular abnormalities could be detected, and the main manifestations were ME, MER, which were hard to be identified under the microscope, leading to failure to adopt reasonable surgical methods, affecting the prognosis of visual function. In this study, 26.7% of dense VH cases whose iOCT results were not consistent with operator’s judgment under the microscope. Based on the results of iOCT scan, a more reasonable surgical method was chosen in 21.6% of cases. All of the 10 cases of MER observed under iOCT scan received an additional ERM peeling and there was no recurrence in the follow-up.
In this study, the iOCT images can clearly display the residual epiretinal membrane, the abnormality of nerve fiber layer and the elevation of the inner retina in the cases of high myopic maculopathy. The qualities of all images were good, confirming the feasibility of iOCT in high myopic maculopathy surgery. Moreover, residual membranes were observed on the iOCT images after the removal of ERMs in some cases, indicating that the application of iOCT can help confirm the integrity of the removal of the membranes during the operation, avoiding the repeated application of dyes during the operation and reducing the possibility of retina toxicity. In addition, in high myopia eyes, the retinal tissues in the macular area are very fragile, and intraoperative damage is more likely to occur. In this study, iOCT can be used to observe micro-damages during the membranes peeling process, such as nerve fiber layer hemorrhage and inner retinal elevation changes. The application of iOCT helps the surgeon adjust the membranes-peeling technique and strength according to the micro-injury during the operation, and reduce the damage to the retinal tissue. The Hole-door phenomenon can also be observed in the iOCT scan results of some patients of high myopia macular hole. Combined with previous research results, the appearance of this phenomenon may indicate a good prognosis, however it needs to be confirmed by a larger sample of clinical trials. Iatrogenic MH is the most serious intraoperative complication of MF. Therefore, it is very necessary to evaluate the presence or absence of MH after ILM peeling, which helps guide the surgeon on what kind of vitreous cavity tamponade to use in subsequent operations. In this study, no full-thickness macular hole was observed in the eyes of MF after ILM peeling, however, one of the eyes was identified as a full-thickness macular hole under iOCT, which played a guiding role in the subsequent selection of vitreous cavity tamponade. Therefore, iOCT can provide more comprehensive information in real time and help the surgeon make further decisions.
Microscope integrated iOCT, as the third-generation iOCT product, has been widely used clinically in a lot of countries, while it has not yet been marketed in China. The vehicle-mounted iOCT used in this study required suspension of surgery for scanning and static image analysis. The average delay time was 3.54 minutes. The DISCOVER study showed that although the microscope-integrated iOCT could perform intraoperative real-time scanning, with the gradual clinical application, nearly 60% of surgeons still preferred the traditional intraoperative static image analysis, which could show a more subtle structural changes than real-time images, and a comparative analysis before and after operation could be conducted.11,12,13 Therefore, the vehicle-mounted iOCT for intraoperative static OCT image analysis still has irreplaceable clinical value. However, with the continuous development and progress of technology, microscope-integrated iOCT will eventually appear and be widely used in the Chinese market. While completing intraoperative real-time scanning, it can also collect and analyze static images at any time during the operation as required. This solves the shortcomings that the vehicle-mounted iOCT needs to suspend the operation and the operation process is relatively cumbersome.
This study has demonstrated both the feasibility and utility of the vehicle-mounted iOCT in Chinese population as it relates to surgical decision-making in vitreoretinal surgery. There are some important strengths and limitations that should be emphasized. The large sample size and dynamic assessment of surgeon impression over time provide enhanced generalizability of the results, the completion of the operation by the same surgeon also reduces the influence of subjective factors on the operation, thereby showing the results more objectively. Important limitations of this study include the lack of control group without the use of iOCT. Moreover, there is a lack of intraoperative fundoscopic imaging as well as the scanning lines show the cross section of iOCT images. Additionally, in this study, only the postoperative BCVA was analyzed as the impact of iOCT on outcomes, but lacked other indicators, such as the integrity of the outer layer of the retina, the thickness of the fovea, the degree of visual deformation, contrast sensitivity, and so on. These may be able to more fully explain the application value of iOCT in vitreoretinal surgery.
In conclusion, the application of iOCT has a significant clinical functionality in vitreoretinal surgery, providing the surgeon with a new surgical understanding, guiding the selection of a more reasonable operative procedure during surgery, predicting postoperative recovery and improving postoperative outcomes.
Conflicts of Interest
The authors declare that there are no conflicts of interest relevant to this article.
Acknowledgments
This work was supported in part by research grants from the Zhejiang Provincial Natural Science Foundation of China (Grant No. LQ19H120003) and National Nature Science Foundation of China (Grant No. 81900910).