Novel intense pulsed light-photodynamic therapy strategy in the treatment of facial actinic keratoses concomitant with rosacea
Abstract
Rosacea presents as transient or persistent erythema, papules, pustules, flushing, and telangiectasia on the middle of the face, which has some clinical similarity with actinic keratosis (AK). These two conditions can coexist in the same patient. Dermoscopy and reflectance confocal microscopy (RCM) could be useful methods for diagnosis and monitoring treatment efficacy. Novel intense pulsed light-photodynamic therapy (IPL-PDT) may have better tolerance and curative effect than traditional red-light 5-aminolevulinic acid photodynamic therapy (ALA-PDT). Herein, we present a case of facial AKs concomitant with rosacea where combination therapy of novel IPL-PDT and oral minocycline was effective in that AK lesions were eliminated and the patient’s facial erythema and telangiectasia were significantly improved.
1. Introduction
Actinic keratosis (AK) is presented as discrete or confluent patches of erythema and scaling, predominantly on sun-exposed skin that usually occurs in middle-aged and elderly people with light pigmented skin. Rosacea is a chronic inflammatory facial dermatosis mainly characterized by persistent central facial erythema, papules, pustules, flushing, and telangiectasia. Rosacea primarily occurs in middle-aged women. Possible pathogenesis involves the dysfunction of neurovascular regulation, abnormal innate immune function, skin barrier dysfunction and D. folliculorum mites.1 Both AK and rosacea can manifest as facial erythema and have been reported to coexist in some clinical cases.2
5-Aminolevulinic acid photodynamic therapy (ALA-PDT) is commonly applied to neoplastic dermatosis such as AK, because of its strong ability to induce cell apoptosis and necrosis.3 As a noninvasive strategy, ALA-PDT is especially recommended in AK patients with multiple lesions and high cosmetic demand.4 Besides the anti-tumor effect, ALA-PDT can be applied to inflammatory skin diseases such as rosacea. Several clinical studies have also confirmed the efficacy of PDT in some cases of rosacea.5
Various light sources can be applied in PDT, including red light and intense-pulsed light (IPL).6 We previously reported that ALA-PDT with traditional red light has strong curative effect but more side effects than other methods.7 Patients with rosacea usually suffer from skin barrier dysfunction, so traditional red light-PDT might cause acute inflammatory reactions like skin irritation. Because IPL with 560–1200nm wavelength is less intensive than traditional red-light illumination, ALA-PDT with IPL might be better tolerated and have less side effects.7 Combining IPL with ALA, may yield synergistic effects for AKs and rosacea as well.
In the following sections, we present a case of a 61-year-old female patient with facial AKs concomitant with rosacea. After three sessions of intense pulsed light-photodynamic therapy (IPL-PDT) treatment together with oral minocycline therapy, the AK lesions were eliminated and the telangiectasia was significantly diminished. No recurrence was observed during 1-year of follow-up.
2. Case Report
A 61-year-old female patient presented with multiple discrete red patches on her face. The patches were approximately 0.5cm in diameter, slightly rough, with indistinct boundaries and covered white scales on the surface of patches. There was no obvious ulceration or erosion on the surface. The skin of the cheeks and nose showed scattered telangiectasia and erythema (Fig. 1(a)). The patient complained noticeable flushing, burning and itching for over 1 year. The flushing and burning sensation are usually aggravated by cold or heat stimulation. Family history of a similar disease was negative. Considering the polymorphism and atypicality of the lesions, dermoscopy and reflectance confocal microscopy (RCM) were used as noninvasive diagnostic strategies. Dermoscopic examination indicated that lesions on the nose had distinct AK characteristics, and both cheeks showed obvious follicular plugging and vascular structures (Figs. 2(a) and 2(b)). In addition, visible structures of Demodex folliculorum were detected in some of the hair follicles by RCM (Figs. 2(c) and 2(d)). In view of the co-existence of AK and rosacea, field-directed traditional ALA-PDT with red light was administered to the patient’s entire face. However, due to obvious skin desquamation, edema and aggravation of erythema after ALA-PDT, we had to adjust the treatment scheme (Fig. 1(b)). We chose IPL with 560–1200nm wavelength as a light source. IPL-PDT was performed for the next three sessions and traditional red-light ALA-PDT was still used for local AK lesions to provide a more intense effect. The patient took minocycline orally (50mg/qn) as a combination therapy during the period time. Due to the photosensitivity of minocycline, the patient was informed to avoid strong sunlight exposure by wearing hat and mask, or using sunshade in the treatment period. After three sessions of IPL-PDT treatment and two months of oral minocycline, AK lesions were fully resolved and the facial erythema and telangiectasia were significantly alleviated (Fig. 1(c)). No Demodex folliculorum was observed with RCM confirmation as of 1 month after the last treatment. There was no recurrence during 1-year follow-up.
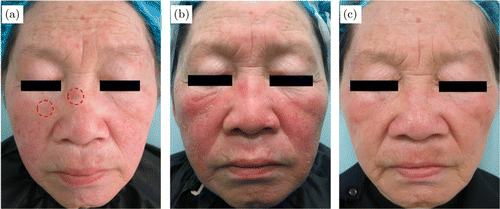
Fig. 1. Clinical images: (a) Before treatment (red circles represent the AK lesions); (b) 1 week after 1 session of ALA-PDT; and (c) 1 year after treatment.
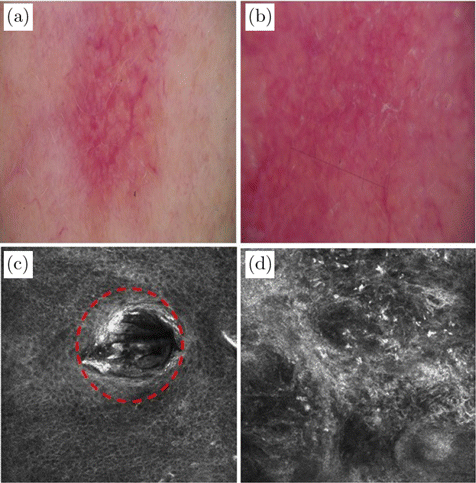
Fig. 2. Dermoscopic image of (a) AK and (b) rosacea. RCM image of rosacea (c) and (d). (c) Disordered honeycomb structure and spongy edema, Demodex folliculorum bodies are visible in the hair follicle (red dotted circle); (d) Highly refractive structures revealing inflammatory cells infiltration.
Traditional ALA-PDT: Freshly prepared 10% 5-ALA cream (Aminolevulinic Acid Hydrochloride Topical Powder, AiLa®, Fudan Zhangjiang, Shanghai, China) was applied to the face and incubated for 3h. The 5-ALA cream was then wiped off and the patient’s face was exposed to a 630nm red light with 100J/cm2 at 100mW/cm2.
IPL-PDT: Freshly prepared 10% 5-ALA cream was applied to the face and incubated for 3h. Then the 5-ALA cream was then wiped off and the whole face was irradiated with 560–1200 nm wavelength IPL (15–17J/cm2 with a spot size of 15×35mm).
3. Discussion
Rosacea can be classified into the following four subtypes: Erythematotelangiectatic (ET), papulopustular (PP), phymatous, and ocular.8 In our case, the patient presented with scattered persistent erythema and telangiectasia on nose and both cheeks, which could be categorized as ET rosacea. The AK lesions were presented as scaly erythema plaques.
Dermoscopy showed strawberry pattern and granular pattern in AK lesions which were diagnostic typical traits. The most common dermoscopic features of rosacea are polygonal blood vessels and orange–yellow areas.9 In our case, dermoscopy only showed follicular plugging and vascular structures but no polygonal blood vessels or orange–yellow areas. The dermoscopy features of the patient’s lesions were not particularly typical and the dermpscopy examination of rosacea is not diagnostic criteria, which mainly depends on clinical features. Surprisingly, the pleomorphic vessels gradually vanished during follow-up visit via dermoscopy examination, suggesting the great benefits of dermoscopy in evaluating efficacy.
In vivo RCM is drawing increasing notice as a noninvasive diagnostic method in dermatology. With RCM, parakeratosis, dilated and crimped blood vessels, and spongiform edema at stratum spinosum can be detected in most rosacea patients. The Demodex folliculorum bodies are also visible in part of the hair follicle. Although the pathogenesis of rosacea is still not fully elucidated, the possible role of Demodex folliculorum in aggravating inflammation through natural or acquired immune response has been reported.10
In ET rosacea, a combination of topical and systemic therapy can be necessary to prevent stubborn flushing and recurrence. Oral minocycline is a standard scheme in the treatment of inflammatory lesions of ET rosacea.11 Although the systemic application of minocycline alleviates the development of inflammation, persistent erythema and telangiectasia resulting from rosacea remains an obstacle.
PDT has antineoplastic, anti-inflammatory, and anti-microbial effects. In the treatment of AKs, PDT causes necrosis or apoptosis in dysplastic cells and influences the tumor immune microenvironment.3 To treat rosacea, vessels can be hardly destroyed by traditional red light-PDT. IPL, a new therapeutic strategy for vascular and pigmented lesions in dermatological clinical settings, can also be used as a light source for PDT with filtered and noncoherent light flashes. Several clinical trials have shown that PDT with IPL is effective in the treatment of AK.12,13,14 It improves photoaged facial skin with fewer side effects compared to other therapy methods. Wang et al. also reported the use of IPL with ALA-PDT in the treatment of acne vulgaris with some surprising effects in modulating the local immune response, increasing skin elasticity, and reestablishing skin barriers.7 In this way, it may be helpful in the management of persistent telangiectasia that accompanies rosacea. The skin barrier of most rosacea patients is impaired to varying degrees, and their skin are easily stimulated with light and heat, so the selection of energy parameters during treatment needs to be extra cautious. Traditional red light-PDT is not suitable for telangiectasia, while IPL shows additional benefits to the dilated blood vessels of rosacea with mild side effects.15
To our satisfaction, our patient displayed better tolerance to IPL-PDT, finding the short-light pulses of IPL less painful than continuous red-light illumination. Some additional synergistic effects such as skin rejuvenation were fostered through the combination of IPL with ALA. For these reasons, IPL-PDT could be a good treatment strategy for facial AKs concomitant with rosacea with satisfactory cosmetic result and good tolerance.
In conclusion, IPL-PDT showed better efficacy and tolerance in the treatment of facial AKs concomitant with rosacea compared to traditional red-light ALA-PDT.
Acknowledgments
This research was financially funded by the National Natural Science Foundation of Shanghai (22ZR1455400), Shanghai Rising-Star Program (20QA1408600), and Shanghai Sailing Program (21YF1441600). Shuzhan Shen and Yajing Cao contributed equally to this work.